A 48 year old man with generalized swelling in legs since 10 days, SOB since 7 days.
A 48 year old man, who works as an auto driver, hailing from Chityala presented to the hospital with-
• generalized swelling of legs since 10 days.
• SOB since 7 days. ( Especially when lying down.)
Date of admission - 21/11/21.
HISTORY OF PRESENT ILLNESS
• Patient was apparently asymptomatic 2 weeks back.
• The patient usually wakes up at around 5am to 6am.
• Then after washing his face and brushing his teeth, he goes out for walking for around 30 minutes.
• After coming back, the patient resumes with his occupation of driving autos till 9pm with a lunch break at 12pm.
• The patient has his food at 9pm and goes to bed early by 10pm.
• Around 10 days back, the patient noticed swelling around his left leg while going on his morning walk.
• The patient also had a general corn inbetween his 3rd and 4th toes, and attributed the swelling to perhaps being that.
• The swelling then appeared on right leg, and then on his two hands all in the span of 3 days.
• Later the patient noticed himself suffer through bouts of fever.
• This prompted the patient to go to an RMP in Nalgonda where he was diagnosed with Pericardial Effusion (minimal) and Pleural Effusion (minimal).
• The doctor prescribed certain regimen of drugs which the patient says has caused him to experience a bad case of shortness of breath.
• The patient also complains of orthopnea since 3 days.
• So the spouse of the patient, decided to stop administering the medication after 3 days.
• He was later brought to this current hospital where he has undergone a dialysis.
• Patient says much of his swelling and symptoms were relieved after dialysis.
PAST HISTORY
• The patient suffers from Diabetes Mellitus since 7 years.
• The patient suffers from Hypertension since 8 years.
• His Hypertension was always apparently under control with medication until his leg swelling, after which it couldn't be controlled.
• 4 years back patient had a incidence of pain in the right hypochondrium - right lumbar region which had an onset on consuming food.
• The patient doesn't suffer from Tuberculosis.
• The patient also doesn't suffer from asthma and epilepsy.
• They were never involved in any kinds of accidents.
• They have never undergone any surgeries.
FAMILY HISTORY
• There is no incidence of similar symptoms in any other member of his family.
• He seems to be the first person to suffer with DM in his family.
• His father has "liver problems" due to the habit of drinking.
• All the deaths in the family except his father's seem to be of natural causes.
• There are no genetic disorders or congenital deformities in his family to his knowledge.
PERSONAL HISTORY
• The patient consumes a mixed diet of vegetarian and non vegetarian food.
• Since his illness, the patient has been only taking vegetarian food.
• The patient recollects that his appetite has been very poor since last 3 days, which was relieved after his first dialysis.
• Patient is obese.
• They appear to be adequately nourished. .
• Gradual decrease in micturition since the onset of illness.
• Bowel movement is constipated.
• They apparently have had the habit of smoking (unspecified quantity), drinking (unspecified amount), and pan chewing since the age of 15 years.
• They have completely ceased from all the above mentioned habits since past 4 years.
ALLERGY HISTORY
• Patient is not allergic to any known drug or food.
• There is no known allergy to dust or pollen in the patient.
DRUG HISTORY
• On equiry, the patient refused to have taken any sorts of steroids, oral diabetes drugs, diuretics, ergot derivatives, monoamine oxidase inhibitors, hormone replacement therapy or contraceptive pills — prior to coming to the hospital.
• The patient is on Insulin and Glimepiride for his DM.
• The patient also takes Olmesartan for his Hypertension.
GENERAL EXAMINATION
• The patient is concious, coherent and cooperative.
• On examination, patient's mood appears to be well.
• Their built is ectomorphic.
• The patient has oedematous face.
• No characteristic gait noted.
• There is no lymphadenopathy present.
• There is presence of clubbing.
• The patient has slight icterus.
• JVP sign unable to notice because of dialysis line insertion.
• There is oedema in both of their legs - pitting type.
• No decubitus sores are present.
• Patient has substantial pallor and pale tongue; appears to be slightly anemic.
• Patient appears to be mildly dehydrated.
• Vitals (on examining)
Temperature- 99.3°F
Respiratory rate- 19 cpm
Pulse Rate- 95 bpm.
S1 and S2 are heard.
spO2- 99%
Blood Pressure is 180/110 mmHg.
PROVISIONAL DIAGNOSIS
Chronic Kidney Disease.
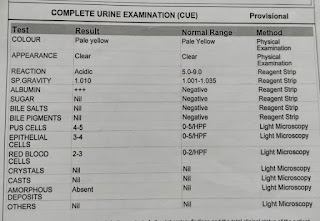
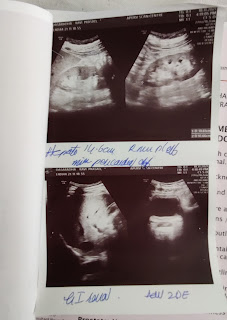
INVESTIGATIONS
FINAL DIAGNOSIS
Chronic Kidney Disease due to Diabetic Nephropathy with Hypertension.
TREATMENT









Comments
Post a Comment